Follow the Money: The SAVE Act
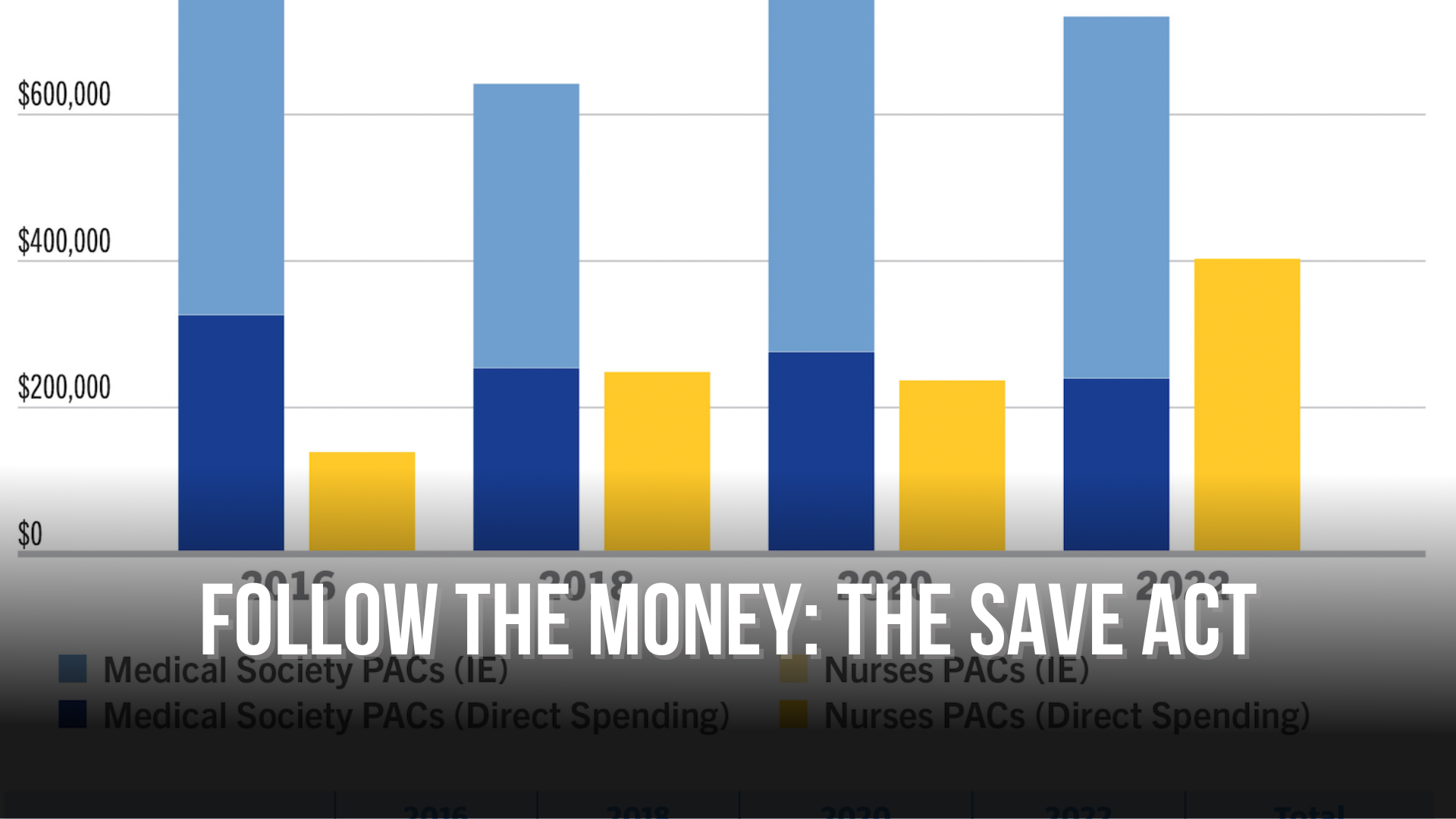
Campaign spending by groups in favor of and opposed to The SAVE Act. Graphic Source: Carolina Journal
By Donna King, Carolina Journal
Stephanie Brinson is an advanced practice registered nurse seeing thousands of patients a year, along with five other APRNs, in a Garner practice open seven days week. They are filling a need for more providers in the state’s healthcare system. However, like other APRNs, Brinson can’t see patients in North Carolina without a “supervising physician.”
Their physician is not part of the daily operations of the office. According to Brinson, the APRNs spend about 15 minutes a year with the supervising physician and pay $30,000 annually for sign-off on their work. If that doctor retires or moves on, they must close their doors until they find another supervising physician.
The SAVE Act, (House Bill 218/Senate Bill 175) filed in the state legislature would change this regulation, allowing nurses like Brinson to practice up to their level of certification, granting them “full practice authority.” More than 25 other states have already passed similar legislation.
“It’s a permission slip to go to work, and more and more people are understanding that the SAVE Act needs to be passed,” said bill sponsor Sen. Gale Adcock, D-Wake, a nurse practitioner herself who has been working to pass the bill for years.
Lawmakers have tried to pass the SAVE Act before without success. With support from Senate Leader Phil Berger, the Senate voted in favor of a similar bill, 44-2, last year, but the House did not take it up. It is a sticking point as lawmakers debate policy on how to increase access to care amid a growing provider shortage and Medicaid expansion, which adds more than 600,000 people to the Medicaid entitlement program.
The issue has generated debate but also big campaign spending. Physicians’ lobbying groups and the North Carolina Medical Society are the primary opponents of the bill and, according to a review of campaign finance reports conducted by Rose Hoban at North Carolina Health News, the eight PACs affiliated with the medical society donated a total of $627,650 to General Assembly candidates in 2022 in the run-up to November’s elections.
EXPANDING NC’S POOL OF PROVIDERS
The SAVE Act is intended to remove regulatory red tape and allow APRNs to practice to the full extent of their training and education. The legislation has a wide range of supporters, including AARP, Blue Cross Blue Shield of North Carolina, Concerned Veterans for America, and Carolina Journal’s founding organization, the John Locke Foundation. There were calls to include the SAVE Act in Medicaid expansion, recently passed by the legislature and signed into law by Gov. Roy Cooper, but it was not.
“Access is a real problem, even in our cities,” said Brinson. “I can’t even begin to imagine the access problems in rural North Carolina where there are no additional people to provide care. Medicaid is going to expand this summer, and I’m excited, but I don’t know who is going to take care of all those people.”
THE DEBATE
Proponents say the SAVE Act is a way to increase the shrinking pool of medical providers and taps a wide range of trained healthcare professionals. Opponents of the bill, like the N.C. Medical Society and N.C. Society of Anesthesiologists, say it risks patient safety.
“The North Carolina Medical Society supports keeping physicians involved in patients’ healthcare,” the N.C. Medical Society said in a statement. “The SAVE Act would remove required physician involvement, allowing patients to be seen by nurses in all circumstances regardless of practice setting or patient’s condition. Eliminating physician involvement in the healthcare team will fracture continuity of care and create risks for patients.”
Rep. Timothy Reeder, R-Pitt, is an emergency room physician and one of the most vocal opponents of the SAVE Act in the N.C. General Assembly.
“Physicians are required to have 10,000 hours of clinical experience, and a nurse practitioner is only required to have 500 hours,” said Reeder. “If they are practicing in a team setting with others, that’s one thing. The educational system for APRNs was not really designed for nurses to practice independently.”
Reeder cited a study by the National Bureau of Economic Research that said nurse practitioners in an emergency setting practicing without medical supervision or collaboration had an 11% increase in hospitalizations. The AMA is actively fighting what it calls “scope creep.”
“In terms of healthcare costs, there are studies that find that while [nurse practitioners] are paid less, they cost more because nurses will order more tests, they aren’t as efficient evaluating patients, have longer inpatient length of stay, and order more consultations,” said Reeder.
Reeder has co-sponsored a separate bill (House Bill 75) that addresses the supervision arrangements for physician assistants. It requires that in a team setting, a practice is majority-owned by physicians that have “consistent and meaningful participation in the design and implementation of health services to patients.” That bill passed the House in February but is sitting in the Senate Rules Committee. H.B. 75 allows for reduced supervision for PAs who practice in a team setting after 4,000 hours of clinical practice experience as a licensed PA and more than 1,000 hours of clinical practice experience within the specific medical specialty of practice.
However, a study from the Center for Growth and Opportunity at Utah State University reports that laws regulating “scope of practice” increase healthcare costs by restricting the supply of providers. A study published by the National Institutes of Health found that states requiring physician oversight of nurse practitioners had a 28% increase in emergency room visits after expanding Medicaid, while states allowing NPs to practice without physician oversight had only a 7% increase.
“It’s not like these 600,000 people haven’t been getting health care. They’ve just been getting it in the emergency rooms, and they’ve been getting it sporadically when they are the sickest and can’t pay for it,” Adcock said. “They need to get care in their communities where it is less expensive, more appropriate — when it will do the most good. That’s where we need not only nurses and midwives, but also pharmacists and physician assistants, working to the top of their license and not restricted by these archaic and patriarchal laws that say you can’t do your job unless some group, who doesn’t know anything about what you do, says you can.”
“It’s not only wrong; it is old-fashioned,” she added.
CAMPAIGN SPENDING
Between the House and the Senate versions, the SAVE Act has 80 co-sponsors, Democrats and Republicans. Sen. Ralph Hise, R-Mitchell, is a regular primary sponsor of the bill, along with Adcock and Sen. Joyce Krawiec, R-Forsyth. Being an advocate for the SAVE Act puts a target on some members when it comes to elections.
In 2022, Hise had nearly $80,000 spent against him in a primary election against Deanna Ballard as independent expenditures (IEs) by NC Citizens for Patient Safety, a political action committee or PAC closely aligned with the North Carolina Medical Society. Both Republicans, Hise and Ballard were “double-bunked” in the last legislative maps. Ballard also received $2,000 in direct contributions from the N.C. Medical Society for the primary. The N.C. Nurses Association made direct contributions to both Hise and Ballard, giving $2,000 to Ballard and $6,600 to Hise in that primary election.
The N.C. Medical Society has spent heavily in favor of Reeder as well, shelling out $276,330.80 of independent expenditures in his race and $23,200 in direct funding to his campaign from the group’s PACs in 2022. Reeder received more than $130,000 from NC Citizens for Patient Safety, a donation that helped him beat Rep. Brian Farkas, a co-sponsor of the 2021 SAVE Act.
*Groups for and against the SAVE Act per the NC Health News report.
“While the Medical Society and its affiliate organizations have outspent nurses nearly three to one on elections, these numbers don’t show the full picture,” said Jim Stirling of the John Locke Foundation. “Anesthesiologists have spent an additional $1.8 million toward General Assembly elections since 2015. When fully accounting the money for and against the SAVE act, this is truly David versus Goliath.”
Despite being outspent by SAVE Act opponents, supporters feel that this session the bill has momentum. Adcock challenged the House leadership to bring it up for a vote.
“I’m finding that more and more people here want to see it passed if only their leadership would let them take a vote,” said Adcock. “Everything looks impossible until it’s inevitable. That’s what happened with Medicaid, and that’s exactly what’s going to happen with the SAVE Act.”
Are you tired of being bombarded by paywalls and pop-up ads when trying to read the news? Do you believe that access to reliable political news should be free and accessible to everyone? Then we urge you to support NC Political News, a weekly electronic political news outlet.
NC Political News is committed to providing high-quality, unbiased political reporting with columnists from all political sides. Unlike other news outlets, NC Political News is free to read and supported by businesses who purchase ad space on our website and in our newsletter, which goes out Monday through Friday at 7:00 am. This means that readers like you can access the news without being asked to pay a cent or dealing with frustrating advertisements.
However, to continue providing this valuable service, NC Political News needs your support. If you believe in the importance of accessible, free news, we urge you to click the image below. Any amount of support is appreciated.
Together, we can keep the news free and help ensure our state stays informed and connected.